What is Chronic Pain?
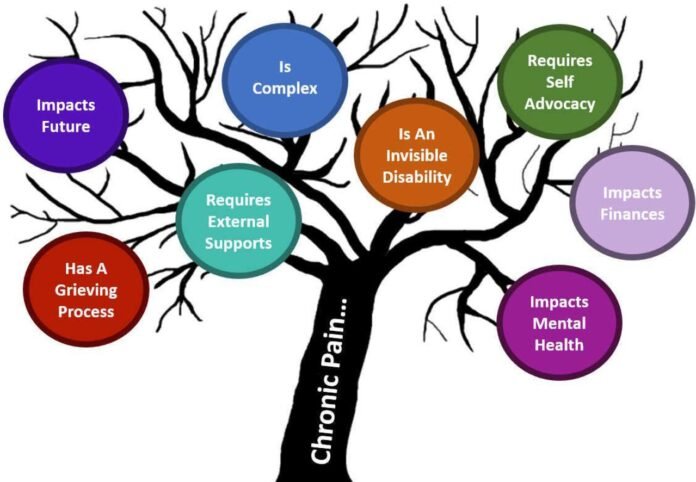
Chronic pain is more than just physical discomfort—it’s a persistent and often unpredictable experience that can color every hour of the day. Defined as pain lasting more than three months, it doesn’t serve the protective purpose that acute pain does, and frequently stays present even after the initial injury or illness has faded. For millions of adults, including nearly 20% of Americans according to the Centers for Disease Control and Prevention, chronic pain can interfere with work, relationships, and simple joys like walking or playing with family. Coping with this invisible burden can become a lifelong learning process, with people constantly seeking new ways to restore movement, comfort, and hope.
Chronic pain comes in many forms, from lingering lower back pain and fibromyalgia to headaches, nerve pain, and joint discomfort from arthritis. While sometimes a specific injury, surgery, or medical condition is responsible, other times the source is unclear, which can add to the frustration. Because chronic pain is so complex, a solution for one person may not work for another. This is why health practitioners and researchers have placed a growing focus on Chronic Pain Treatment approaches that address the unique challenges of each individual. The shift isn’t just about reducing pain and restoring confidence, independence, and a sense of control over daily life.
Modern Methods for Pain Management
Managing chronic pain today involves far more than prescribing painkillers. While medications can still play a helpful role—especially for short-term flare-ups—doctors are increasingly turning to multidisciplinary plans that blend physical, emotional, and medical support. In most settings, physical therapy is foundational, offering personalized movement programs to gradually restore strength, flexibility, and confidence in using the body. Occupational therapists can also teach new ways to accomplish necessary tasks, reducing strain and preventing further injury. Injections, nerve blocks, TENS (transcutaneous electrical nerve stimulation), and ultrasound treatments give targeted relief for specific issues, helping people get “over the hump” of severe pain episodes without heavy medication reliance.
The most successful outcomes often come from working with a team. By involving doctors, physical therapists, pain specialists, nutritionists, and psychologists, individuals benefit from regular check-ins and tailored adjustments to their plan. This flexibility is especially crucial since the nature of chronic pain can change over time. Adding or removing strategies based on ongoing assessment keeps people engaged and in tune with their bodies, rather than feeling trapped by a one-size-fits-all regimen. The empowerment and encouragement found in modern team-based care can give people the resilience they need to keep moving forward.
Integrative and Alternative Strategies
Beyond the doctor’s office, integrative and alternative methods have carved out a strong presence in the world of pain management. For many, these therapies aren’t just add-ons but essential pillars in a personal toolbox. Acupuncture, long practiced in Eastern medicine, has captured interest in Western research for its ability to relieve chronic pain. The National Institutes of Health highlights promising results for people with back pain, migraines, osteoarthritis, and other conditions. By targeting specific points in the body, acupuncture stimulates the nervous system and promotes the body’s natural healing response.
Other alternative approaches like massage therapy, chiropractic adjustments, and gentle exercise methods—think yoga, tai chi, or Pilates—are widely used for their ability to reduce muscle tension, improve circulation, and bring about a more profound sense of relaxation. Patients often need to experiment to discover which combination helps them most. Real-world stories reveal that small, steady additions, such as attending a weekly yoga class or scheduling periodic therapeutic massage, can significantly shift pain levels, mood, and mobility. Instead of searching for a “magic bullet,” integrative strategies are about layering small, manageable practices that create a foundation for sustained relief.
The Role of Mind-Body Connection
The relationship between the mind and body is central in pain science. Researchers now understand that the brain can both amplify and quiet pain signals. Practices like mindfulness meditation, deep breathing, and progressive muscle relaxation teach people to focus on the present moment and disengage from the spirals of worry or fear that can heighten physical suffering. Cognitive-behavioral therapy (CBT) has particularly robust evidence for helping people reframe negative thoughts related to pain, replace unhelpful coping habits, and build up a sense of mastery over their situation.
People often notice that when anxiety and tension drop, so do pain levels. For instance, when a migraine sufferer learns to recognize early stress signals and use mindfulness to calm themselves, they may find their headaches become less frequent or intense. These mind-body practices are not just for symptom management—they can lead to lasting changes in how pain is experienced. The result is a toolkit that helps manage pain, sleep, mood, relationships, and even the motivation to participate in life’s daily routines.
Lifestyle Habits to Support Relief
- Regular Physical Activity: Even if movement starts gently, maintaining some degree of exercise can help reduce inflammation, increase endorphins (the body’s natural painkillers), and protect joints from stiffness. Whether it’s aquatic therapy for joint pain or light cycling for back issues, the key is persistence and gradual progress.
- Balanced Nutrition: Diets rich in leafy greens, berries, healthy fats like olive oil and fish, and moderate amounts of lean protein support anti-inflammatory processes. Avoiding processed foods, excess sugar, and high-fat animal products can further reduce triggers for pain flare-ups.
- Structured Sleep Patterns: Poor sleep both increases pain sensitivity and slows recovery. A regular bedtime, minimizing screen time before sleep, and keeping the bedroom cool and dark can help reinforce the body’s healing rhythms.
- Stress Reduction: Simple daily practices like box breathing, creative hobbies, or guided meditation lower overall stress, quieting the nervous system’s pain alarm.
Many who have lived with chronic pain for years say that it’s the everyday routines—not major overhauls—that genuinely make a difference. Tracking triggers and responses in a journal, celebrating minor improvements, and focusing on what can be controlled empower people to move forward even when pain is a constant presence.
Psychological Support and Counseling
The intersection between emotional well-being and chronic pain is powerful. Long-term discomfort can lead to anxiety, depression, irritability, and sometimes isolation from friends and loved ones. Regular psychological support, whether through counseling, therapy, or participation in support groups, offers space to process frustrations, fears, and changes in self-identity that can come with chronic conditions. Structured therapy sessions provide validation and new coping skills, while group discussions break down the walls of loneliness and offer practical ideas from those who understand firsthand.
By weaving mental health support into pain management, people can better handle setbacks, maintain hope during tough stretches, and find new motivation to try solutions. Therapists and support groups not only provide immediate relief but can also be vital resources when pain impacts work, family, or personal goals.
Future Directions and Research
The landscape of chronic pain care constantly evolves as new research opens doors to innovative therapies. Exciting technological developments—such as wearable devices for nerve stimulation, apps for pain tracking, and virtual reality for distraction—are making it possible to customize treatment like never before. Researchers are also investigating regenerative treatments, such as stem cell injections and gene therapies, that could one day address pain at its root source rather than just masking symptoms.
Scientific coverage frequently spotlights breakthroughs in how chronic pain alters the body and brain, fueling the possibility of truly personalized medicine. Future medical teams may use a blend of genetic data, wearable technology, and detailed patient tracking to fine-tune care for each person. News stories underscore the importance of a holistic approach—one informed by the latest science but always centered on individuals’ lived experience and preferences.
FAQs: Common Questions Answered
- Is chronic pain ever fully curable? While complete cures remain elusive for many, almost everyone can find significant relief and an improved quality of life by combining approaches tailored to their circumstances. The goal shifts from total elimination to effective, sustainable management.
- Can simple lifestyle changes help? Yes. Decades of clinical evidence support that physical activity, good nutrition, and effective stress relief boost resilience and often reduce pain by noticeable margins over time.
- How should someone choose an integrative approach? Collaboration is key. Exploring possible options with doctors, pain specialists, or therapists and slowly adding what feels safe and helpful leads to the best results. Being open to trying new techniques while letting go of what doesn’t work keeps the plan sustainable.
- Are these therapies right for everyone? Every person’s experience of pain is unique. Some approaches may fit better for specific conditions or lifestyles, so it’s vital to tailor changes to your body and consult with healthcare professionals, especially when adding new or unfamiliar therapies.